- Anterior chamber
- Cornea
- Suspensory ligament
- Ciliary body
- Sclera
- Choroid
- Vitreous chamber
- Optic disc
- Retina
- Lacrimal gland
- Eyelid
- Pupil
- Iris
- Lens
anatomy and terms | eyelids | entropion | ectropion | glaucoma | conjunctivitis | abrasions, lacerations | ulcerative keratitis | pinkeye | cataract | uveitis | eye medications
Introduction: It is important to examine an animalís eyes on a routine basis. Repeated examination allows one to become familiar with the normal appearance of the eye, so any abnormalities will be noticed immediately. Signs of an eye problem vary tremendously and may include cloudiness, tearing, squinting, discharge, redness, blinking, swelling, an increase in blood vessels, or changes in the size or shape of the pupil. Some animals may rub the eye in an attempt to relieve irritation and itching. Any change in the eye or surrounding tissue may signal a problem and should be a cause for concern.
Many different problems can result in the same set of disease signs, so diagnosis cannot be made by clinical signs alone. Physical examination and special tests are needed to properly identify the cause of most problems. Tests may include a fluorescein dye test, a Schirmer tear test (testing for tear production), tests to measure pressure within the eyeball, and ocular examination with different types of lenses. The eye may be dilated to allow for proper visualization of the back of the eye.
Eye problems should be brought to the attention of a veterinarian immediately. Prompt diagnosis and treatment can prevent further eye problems that can lead to loss of sight. In addition, changes in the eyes may be a sign of whole body disease. By immediately identifying and reporting any changes, diseases can be diagnosed early and treatment can begin.
Although all eye problems should be reported to a veterinarian, it is important for the sheep or goat owner to identify and recognize common eye ailments. The eye is composed of several parts, all of which can be injured or become diseased. Eye problems and diseases can affect one portion of the eye or simultaneously be found in several areas of the eye.
Basic Anatomy and Terms: The eye is protected by upper and lower lids, as well as a third eyelid, called the nictitating membrane. Glands which produce tears are located under the lids. The front portion of the eye itself is covered with a thin, clear covering called the cornea. The remainder of the eye is covered with dense white tissue, the sclera. The margin of the cornea and the sclera is called the limbus. The episclera is the outside surface of the sclera. The conjunctiva is the tissue which reflects from the inside of the eyelids onto the globe. Glands which produce tears are also located in the conjunctiva.
The iris is the colored portion of the eye; the black open space in the iris is the pupil. Behind the pupil is the lens. The lens is attached to the ciliary body. The back of the eye is covered with a layer of tissue called the retina. The inside of the globe is filled with a clear fluid called aqueous humor. This fluid is produced by the ciliary body and nourishes the eye while helping to maintain its shape. This fluid is continually produced and drained from the eye. Drainage occurs at the iridocorneal angle, also called the drainage or filtration angle.
Glossary of Eye Terms:
Figure #1: Vertical cross-section of
the eye .
|
 |
Copyrighted graphic used by permission from
Anatomy of Domestic Animals, Sudz Publishing (email: sudzpub@mac.com)
Introduction:
Sheep and goats have three eyelids. The upper and lower lids help to protect the eye from the environment, distribute tears over the entire eye surface, and control the amount of light that enters the eye. The third eyelid is located in the inner corner of the eye and sweeps across the eye as it closes. It functions to protect and lubricate the eye. It has its own set of tear glands that produce lubricating tears for the entire eye.Problems with the lids can result in pain, swelling, redness, excessive tearing, and drainage from the eye. Animals with lid pain may attempt to rub their eyes, squint, and show other signs of pain. Problems with the lids can lead to additional problems with closely associated structures such as the cornea, conjunctiva, and nasolacrimal drainage system of the eye.
Nasolacrimal Duct System and Lacrimal System
Introduction: The lacrimal and nasolacrimal duct system function together to ensure that the eye is continuously bathed in protective tears and that the tears are removed from the eye. The lacrimal system is responsible for the production of tears. Glands in the eye produce tears that act to lubricate the eye and cornea, protect the eye from environmental debris, supply nutrients to the eye, and wash away irritants. Both the lacrimal glands and the gland of the third eyelid contribute to tear production. After the tears protect and bath the eye, they are drained via the nasolacrimal system. This duct system is responsible for drainage of tears from the inner corner of the eye into the inside of the nose. Health of the cornea and conjunctiva depends on the continuous production of tears and their uninterrupted removal from the eye.
If there is a problem with any part of the system, drainage of tears from the eye may be impeded. If the tears do not drain into the duct system, they will spill over onto the face, creating a condition called epiphora. Signs include wet facial hair and skin.
Problems Associated with the Nasolacrimal System
Obstruction of the Puncta or Ducts: One of the most common causes of nasolacrimal duct problems in sheep is caused by nasal bot larvae. Nasal bot larvae normally reside in the sinuses of the sheep. Occasionally, one of these larvae will migrate up the nasolacrimal duct and cause a blockage. Animals with a blockage of the duct will have tears that spill over onto the face (epiphora) and they may experience conjunctivitis. General nasal bot infections cause the animal to sneeze and have a nasal discharge. Treatment for this problem includes removal of the bot larvae from the duct, along with flushing of the duct. Oral ivermectin is also necessary.
Other causes of obstructions may include inflammation that closes down any
part of the duct system. This obstruction can be caused by conjunctivitis or by
physical irritants such as sand, plant stems, and other foreign objects.
Diagnosis is based on ocular examination and appropriate testing. Treatment
would include antibiotic and anti-inflammatory medical therapy, removal of any
foreign objects, and flushing of the duct system.
Problems with the Eye and Associated Structures:
Globe or Eyeball
Conjunctiva
Introduction:
The conjunctiva is the membrane that lines the inside of the eyelids and the third eyelid, and covers the outside of the sclera. The conjunctiva is a mucous membrane with an excellent blood supply. It connects the lids to the globe and contains specialized glands. These glands produce the inner layer of the tear film.Problems affecting the conjunctiva may be limited to only the conjunctiva or
may involve other portions of the eye. Conjunctival inflammation or disease may
also signal illness that affects the entire body. It is important to recognize
whether disease processes are limited to the conjunctiva, extend to other parts
of the eye, or signal whole body (systemic) disease.
Cornea
Introduction:
The cornea is the outer, transparent layer of the front of the eye. It protects the eye while still allowing light to pass through. The cornea is protected by a layer of tears and by continuously replacing its superficial cells. It lacks blood vessels (which helps make it transparent), and so does not heal easily. Any disease process or insult to the cornea can result in cloudiness, swelling, or pigmentation, which in turn may lead to loss of vision. Corneal irritation or inflammation is extremely painful. It is critical to treat any corneal problem as rapidly as possible.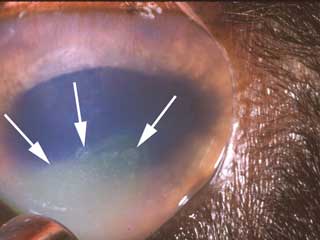 |
|
Treatment depends on the severity, depth, and age of the wound. Care should be
taken to apply only minimal pressure to the face and eye to prevent rupture of
the eyeball. Any foreign body should be flushed out, removed with a dampened
cotton-tipped applicator, removed with forceps, or surgically removed from the
eye. Superficial wounds can be treated with topical medications to prevent
infections and calm the eye. Topical eye medications include antibiotics and
atropine.
Extensive corneal lacerations and corneal penetrations require surgical
repair. Surgical repair will also be needed for those injuries that contain a
foreign body that is not easily removed. All corneal wounds should be
rechecked at specific intervals to monitor healing. Superficial wounds can be
checked at 3 day intervals; deep wounds should be checked daily for the first
several days.
Prognosis depends on the extent of the wound and the time elapsed between
injury and veterinary treatment. The deeper the wound, the poorer the
prognosis. Most superficial corneal abrasions and wounds heal quickly and
satisfactorily. Deeper wounds or those created by blunt trauma may result in
permanent loss of vision, inflammation, and pain. The full extent of the
damage caused by the wound may not be apparent for days to weeks following the
injury, so re-examination is necessary.
 |
|
Diagnosis is based on ocular examination and fluorescein dye testing. If
needed, specific examination of the interior of the eye and cytology can also
aid in the diagnosis. Other tests, such as a Schirmer tear test, are performed
to rule out additional or contributory eye diseases.
Treatment involves elimination of the cause, along with specific treatment for
the ulceration and inflammation. Underlying eye problems, such as
keratoconjunctivitis, entropion, or ectropion, should be treated
appropriately. Treatment of the ulcer may include topical antibiotics to
prevent infection, topical atropine to control pain, specific medications to
control fungal or viral infections, and if indicated, specific medications to
prevent collagen breakdown. Animals may be placed on systemic non-steroidal
anti-inflammatory (NSAIDs) medications such as aspirin or banamine.
Some ulcers are treated with protective contact lenses. Others may require
surgery to trim (debride) the ulcer edges. Additional surgical procedures
include punctuate keratotomy, conjunctival flaps, and flaps created from the
nictitans. Eyes should be rechecked at approximately 3-day intervals; those
with deep ulcers should be rechecked daily until satisfactory healing is
observed.
The prognosis for ulcerative keratitis depends on the underlying cause, the
severity of the ulceration, the type of treatment employed, and response to
therapy. Simple, superficial ulcers often heal nicely in approximately 1-2
weeks. Deeper ulcers treated with surgical techniques may require 4-6 weeks to
heal; those treated without surgery may take longer, or never heal
satisfactorily. Refractory ulcers may remain unhealed for months unless
treated with surgical techniques. After surgery, healing may occur in 2 weeks,
and conjunctival flaps may be left in place for a month or longer. Untreated
or incorrectly treated corneal ulcers can progress, resulting in rupture of
the cornea and loss of vision. This often results in removal of the globe.
Figure #4: This is an example of keratoconjunctivitis (pinkeye) in a sheep.
Lens
Introduction:
The lens focuses light waves that come through the pupil. It is held in place by small suspensory ligaments called lens zonules that attach the lens to the ciliary body. The ciliary body can contract and relax, thereby changing the shape of the lens. The changing shape of the lens allows it to properly focus light waves from different distances onto the retina.Cataract: Cataracts are the most common lens problem in sheep and goats. Cataracts refer to either opacities within a lens or an entire lens that is opaque. The term cataract means "to break down," referring to the loss of normal architecture of the fibers in the lens or its capsule, resulting in an increase of fluid in the lens and loss of transparency. Cataracts are hereditary in many breeds of sheep and goats, and are often present at birth.
Although most cataracts are hereditary, other factors can contribute to the formation of cataracts. These can include metabolic diseases, trauma to the globe, exposure to toxins, and inflammatory diseases such as uveitis. Diagnosis is made by examination of the eyes. Cataracts can be classified by location in the lens and degree of development. Examination of the retina should accompany any examination for cataracts.
Treatment is reserved for cataracts that cause blindness. There is no effective medical therapy. Treatment involves surgical removal of the lens. Because of the complicated and expensive nature of this surgery, it is not commonly done in large animals. Although several techniques can be used, phacoemulsification is commonly used today. This technique involves the use of a small ultrasonic probe that is placed into the eye. It shatters the cataract and then removes the broken-down debris by suction.
Uvea
Introduction:
The uvea is a very vascular structure that is critical for the maintenance of a healthy eye. It is a pigmented, vascular tunic that sits between the outer fibrous layer of the eye (cornea and sclera) and the inner nervous layer (retina). It is comprised of 3 connected portions - the iris, the ciliary body, and the choroid. The anterior uvea is made up of the iris and the ciliary body. The posterior uvea, located towards the back of the eye, is comprised of the choroid. The iris controls the amount of light that enters the eye. The ciliary body controls the focus of the lens, produces aqueous humor, and helps regulate intraocular pressure. The anterior uvea acts as a blood-aqueous barrier and prevents unwanted particles from the bloodstream from entering the aqueous humor. The choroid provides nourishment to the retina, and most diseases of the choroid are linked to disease of the retina.Because the uvea is highly vascular, it is very reactive to changes in the body and is easily inflamed. Inflammation of the uvea is called uveitis. Specifically, inflammation of the iris and ciliary body is termed anterior uveitis. Posterior uveitis refers to inflammation of the choroid. Inflammation may be limited to only the anterior or posterior uvea, or involve both portions. Inflammation of the uvea allows particles to cross the blood-aqueous barrier and enter the aqueous humor. This causes an inflammatory response in the aqueous which can lead to a reduction or total loss of vision.
Uveitis: Inflammation of the uvea may occur with several disease conditions seen in the eye. The cause may be external to the eye and include trauma. In addition, uveitis may follow corneal injuries and corneal ulceration. Uveitis in sheep and goats is most often caused by infectious agents such as Mycoplasma, Listeria monocytogenes, Chlamydia psittaci, and Toxoplasma gondii. These infections can be limited to the eye or cause disease throughout the body.
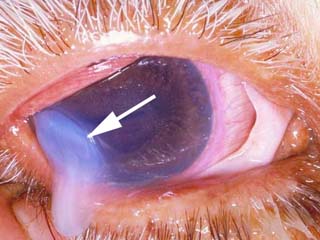
Signs of uveitis may include pain, redness of the conjunctiva, corneal edema, red blood cells or white cells in the anterior chamber, epiphora, spasm of the eyelids, and aversion to light. Other ocular changes are specific to anterior uveitis. These include constriction of the pupil, a change in the color of the iris (often darker), swelling of the iris, and enlargement and engorgement of deep blood vessels located in the ciliary body. In addition, inflammatory cells and pigment may clump together and adhere to the cornea, forming small, visible masses called "keratic precipitates." As particles form or flood into the inflamed area, the aqueous humor becomes turbid. This condition is referred to as "aqueous flare." In chronic cases, the iris may actually adhere to the lens, "fixing" the pupil in an unmovable position. This results in a distorted and immobile pupil. Finally, uveitis can be associated with other serious eye problems, including cataracts, ulcerative keratitis, and secondary glaucoma.
 |
|
 |
|
Diagnosis is based upon complete physical and ocular examination. A thorough eye examination includes measurement of the intraocular pressure. The pressure is typically decreased with uveitis. Additional testing may include blood testing and urinalysis to search for the underlying cause of the disease.
Treatment is aimed at reducing the inflammation of the uvea while determining and eliminating the underlying cause. Anti-inflammatory agents including corticosteroids (1% prednisolone acetate, 0.1% dexamethasone) and non-steroidal anti-inflammatories can be applied topically. Topical medications that dilate the pupil are also used (atropine). In some cases, corticosteroids can be injected under the conjunctiva or administered systemically. Treatment may be altered depending on the cause of the uveitis and the systemic illnesses that are present. Treated animals should be re-examined within one week following the initial treatment and re-evaluated every few weeks.
Prognosis depends on the severity of the uveitis at the time of treatment and
the underlying cause of the uveitis. Early, aggressive treatment of the uveitis
and the initiating cause is necessary to prevent secondary problems. Prognosis
is good if the underlying cause is identified and eliminated, and appropriate
eye therapy is instituted. If uveitis is left untreated, glaucoma, lens luxation,
and blindness can result. Successful treatment can involve several months of
continual medication and follow-up examinations.
Introduction:
The retina is the back portion of the eye. It is considered the "film" that records the visual images that come through the cornea and are focused by the lens. The cells of the retina receive the light images. These cells are of two main types, rods and cones. The rods are sensitive to dim light and the cones are sensitive to bright light. The rods are useful at dusk, while the cones perceive images in the day and help distinguish colors.The rods and cones translate the light images into chemical messages which affect adjacent nerve fibers. The retinal nerve fibers converge together at an area called the optic disc to form the optic nerve. The messages travel as nerve impulses along the optic nerve to the brain where they are again converted into visual images. Any type of damage to the retina will result in interruption of this process and cause loss of vision.
Degeneration of the Retina: If the retina degenerates or atrophies, messages from the eye will no longer reach the brain and blindness will result. Conditions such as trauma, infection, neoplasia, retinal detachment, malnutrition, glaucoma, and inflammation can lead to degeneration of the retina. In many cases, retinal degeneration is a primary condition that is inherited in certain breeds of sheep and goats (South Hampshire sheep and Toggenburg goats).
Infections of Listeria monocytogenes, Toxoplasma gondii, Elaeophora schneideri, scrapie, and the bluetongue virus can all cause inflammation and problems in the retina. Vaccinating ewes with a modified live bluetongue vaccine during the first half of gestation can also cause retinal damage to their lambs. Animals that continually graze bracken fern (causing "bright blindness") or locoweed can develop retina problems. Deficiencies in vitamin A can also cause the retina to degenerate.
No matter the exact cause of retinal degeneration, the signs of retinal degeneration are often the same. In the early stages of retinal disease, the animal may not show many signs. As the retinaís cells degenerate, the animal loses vision. For animals that consume toxic plants such as bracken fern, the loss of vision may not appear until several months after starting to consume the toxic plant on a regular basis. Similarly, animals that are being fed a diet that is deficient in vitamin A will not usually show any signs for at least 3 to 7 months. Affected animals typically lose night vision first ("night blindness"). These animals may have difficulty seeing in poorly lit areas or at night. Eventually, the retinal atrophy will progress, and total blindness will result. An owner may be aware of dilated pupils or a shine from the back of the dilated eye, or may notice nothing until the animal has totally lost vision. Some animals may develop other eye changes, such as cataracts. Many animals will not eat and begin to lose weight and condition.
Diagnosis is based upon ocular examination. Pupils will be dilated and non responsive to light. The retinal area will be hyperreflective and retinal examination will show degeneration of the retina and optic nerve, along with changes in the retinal blood vessels and pigmentation.
In many of these cases, if the animal is completely blind, there is no treatment. Once damage has been done to the retina and surrounding structures, it cannot be reversed. However, for cases of vitamin A deficiency, where the animal only experiences "night blindness," placing the animal on vitamin A supplements and allowing the animal access to plenty of green forage can reverse the problems. Vitamin A can be given as an injection or as an oral supplement. Non-lactating animals should receive 45-50 international units (IU) of vitamin A per kg of body weight per day. Lactating or pregnant animals may require up to 85 IU per kg per day. Animals that are grazing bracken fern or locoweed should be denied access to the plants. This may not reverse any damage already in place, but it will help prevent continued injury. Animals that have a hereditary form of retinal disease should not be used for breeding purposes.
Eye Medications: Eye medications can be delivered by several methods.
Topical medications are applied directly to the eye surface. The topical
medications may be available as eye drops and ointments. This method of
administration is appropriate for both hospital and home treatment of eye
diseases in sheep/goats. In addition, veterinarians may administer medications
via injection into the eye. Common sites for these injections are
subconjunctival (beneath the conjunctiva), retrobulbar (behind the eye), or
intraocular (into the eyeball).
In addition, diseases of the eye may be treated with medications that are given directly to the animal, either by mouth or by injection. Finally, eye diseases may not be limited to the eyes; they may be a sign of disease that is affecting the entire body. In this case, the veterinarian will prescribe medication to treat the primary illness, as well as to control the problems in the eyes.
The following tables list commonly used eye medications. Depending on the combination of related eye problems present at one time, a specific medication may need to be combined with other medications or may be inappropriate for its original, intended use. All eye medications should be used under the guidance of a veterinarian. Page C220 of this manual has information on how to properly clean the eye and administer products.
| CLASSIFICATION/USE/INDICATION | MEDICATION | SPECIFIC USE NOTES | CONTRA-INDICATION (IF ANY) |
| EYE RINSES
USE: Clean, rinse, flush INDICATIONS: Clear mucus before instilling medications, remove debris
from eye |
Sterile, buffered isotonic solutions containing sodium chloride, sodium citrate, sodium phosphate | ||
| Combinations of water, boric acid, zinc sulfate | |||
| EYE LUBRICANTS USE: Lubricate, prevent eye irritation, relieve dryness INDICATIONS: Whenever general anesthesia is used, keratitis, ectropion |
Pilocarpine | Irritating, can cause conjunctivitis and worsen uveitis, not commonly used | Can affect respiration and cardiac function |
| Polyvinylpyrrolidone | |||
| Polyvinyl alcohol | |||
| Methylcellulose | |||
| Ethylene glycol polymers | |||
| Refined petrolatum | |||
| Refined lanolin | |||
| Refined peanut oil | |||
| MUCOLYTICS
USE: Prevent collagen break-down, break up mucus INDICATIONS: "Melting" corneal ulcers, chronic conjunctivitis,
keratoconjunctivitis |
Acetylcysteine | Very expensive | |
| Autologous plasma | Sometimes used in place of acetylcysteine | ||
| ANESTHETICS
USE: Topical pain relief INDICATIONS: Minor surgery, eye examination, diagnostic procedures,
preoperative evaluation of entropion, removal of foreign bodies |
Proparacaine 0.5% | Never use therapeutically. May cause corneal irritation. | |
| Tetracaine HCl 0.5%* | |||
| ANTIBIOTICS (SINGLE)
USES: Preparation for an intraocular procedure. Treatment of infection (if possible, select specific agent for microbe; if testing is not possible, broad spectrum or combination antibiotic is preferred.) Preventive pre and/or post-procedure. INDICATIONS: Treat susceptible infections contributing to uveitis, conjunctivitis, blepharitis, keratitis. Control secondary bacterial infections in conditions such as proptosis of the globe, entropion, ectropion, corneal ulcer, corneal abrasion. |
|||
| Gentamicin 0.3% solution and 0.3% ointment | Susceptible bacteria may include Staphylococcus, Corynebacterium, Pseudomonas, Proteus spp, Escherichia coli, Hemophillis, Enterobacter, Moraxella | ||
| Tetracycline 1% solution and 1% ointment | Susceptible bacteria may include Staphylococcus, Corynebacterium spp,, Hemophillis spp, Moraxella, Chlamydia, Mycoplasma spp | ||
| Tobramycin 0.3% solution and 0.3% ointment | Susceptible bacteria may include Pseudomonas, Proteus spp, Escherichia coli, Hemophillis, Enterobacter, Moraxella, Staphylococcus | ||
| Bacitracin 500 U/g ointment | Susceptible bacteria may include Staphlococcus, Streptococcus, Corynebacterium spp | ||
| Chlortetracycline 1% ointment | |||
| Erythromycin 0.5% ointment | |||
| Neomycin 0.35% ointment | Susceptible bacteria may include Staphylococcus, Corynebacterium spp, Hemophillis spp, Moraxella, Enterobacter, Mycoplasma | ||
| ANTIBIOTICS (COMBINATION)
USE: Same as single antibiotic When more than one type of microbe is present or when testing for specific identification is not possible. INDICATIONS: Same as single antibiotic |
Neomycin sulfate, Polymyxin B sulfate solution and ointments | ||
| Neomycin sulfate, Polymyxin B sulfate, gramacidin solution | Preferable drug for broad spectrum coverage without culture/sensitivity | ||
| Neomycin sulfate, Polymyxin B sulfate, Bacitracin ointment | Preferable drug for broad spectrum coverage without culture/sensitivity | ||
| Oxytetracycline HCl, Polymyxin B ointment | |||
| ANTIINFLAMMATORY - STEROIDAL
USES: All allergic ocular diseases. Nonpyogenic inflammations of any ocular tissue. Reduction of scar tissue. Certain ocular surgeries. INDICATIONS: Blepharitis, conjunctivitis, proptosis of the globe, uveitis,
entropion, chronic superficial keratitis |
Prednisolone acetate suspension | Avoid when there is no specific indication for
steroid use.
Contraindicated in the treatment of corneal ulceration, viral infection, & keratomalacia. May promote fungal infections. |
|
| Dexamethasone | |||
| Triamcinolone (topical and injectable) |
|||
| Betamethasone (topical and injectable) |
|||
| Methylprednisolone acetate (injectable) | |||
| ANTIBIOTIC/STEROID COMBINATIONS
USES: Control inflammation and bacterial infection, treat acute and chronic inflammatory processes of the eye INDICATIONS: Acute or chronic conjunctivitis, inflammation of the anterior segment of the eye, blepharitis, conjunctivitis, proptosis of the globe, entropion, uveitis |
Neomycin sulfate, Polymyxin B sulfate, Dexamethasone solution and ointment | Commonly used | Any condition in which corticosteroid use is contraindicated |
| Neomycin sulfate, Hydrocortisone acetate solution and ointment | |||
| Neomycin sulfate, Zn bacitracin, Polymyxin B sulfate, Hydrocortisone ointment | Commonly used | ||
| Neomycin sulfate, Polymyxin B sulfate, Hydrocortisone solution | |||
| Neomycin sulfate, Prednisolone solution & ointment | |||
| Neomycin sulfate, Dexamethasone phosphate solution | |||
| Neomycin sulfate, Methylprednisolone ointment | |||
| Gentamicin with Betamethasone | Commonly used | ||
| TOPICAL NON-STEROIDAL ANTI-INFLAMMATORY
USE: Reduce inflammation and pain INDICATIONS: Uveitis, cataract surgery, panophthalmitis, corneal ulcers |
Flurbiprofen | May delay corneal healing | |
| Suprofen | |||
| Diclofenac | |||
| MYDRIATICS
USE: Dilation of the pupil (mydriasis), control ciliary spasm and the accompanying pain which causes eyelid spasm, photophobia, and lacrimation INDICATIONS: Non-surgical treatment axial cataracts. Preoperative mydriasis for cataract surgery and
other ocular surgery, corneal abrasions, corneal ulceration, keratitis,
anterior uveitis, possibly proptosis of the globe. |
Atropine sulfate | Not for routine eye examination | May compromise tear production. May predispose to local irritation. Contraindicated in glaucoma or in animals predisposed to glaucoma. |
| Tropicamide | Short-acting - used for eye examinations | ||
| Phenylephrine HCL | Combined with atropine | ||
| MIOTICS
USE: Cause contraction of the pupil, enhance aqueous outflow INDICATIONS: Keep luxated lens in posterior chamber, treat glaucoma |
Demecarium bromide | Cholinesterase inhibitor, do not use with organophosphate insecticides | |
| Pilocarpine | May irritate the eye | ||
| Carbachol | All miotics are contraindicated in glaucoma secondary to anterior uveitis | ||
| ADRENERGICS
USE: Lower intraocular pressure. Control capillary bleeding during surgery INDICATIONS: Control/treat glaucoma |
Epinephrine | Adrenergic agonist/increases outflow of aqueous humor | |
| Timolol maleate | Beta blocker/ Reduces aqueous formation | ||
| CARBONIC ANHYDRASE INHIBITORS
USE: Decrease aqueous humor production INDICATIONS: Control/treat glaucoma |
Acetazolamide (given orally) |
May cause metabolic acidosis and electrolyte imbalances | |
| Methazolamide (given orally) |
|||
| Dichlorphenamide (given orally) |
Use with caution in animals with sulfonamide sensitivity | ||
| Ethoxzolamide (given orally) |
|||
Summary: The eye is a complex structure that processes images for transfer to the brain. It is composed of several interrelated structures. A problem that affects any portion of the eye can result in loss of vision. A problem that affects one portion of the eye may also affect adjacent structures. Because different disease processes can cause the same signs in the eye, examination by a veterinarian is necessary for proper diagnosis and treatment. Prompt examination and treatment can prevent severe, progressive disease. Animals should be examined by a veterinarian at the first sign of any eye problem.
* All of the pictures were used with permission from Colorado State University Ophthalmology Service.